As an expert consultant, I can ensure that you would cover your drug and alcohol rehab by Medicaid. Only if you truly need the financial support. Even in recent years, Medicaid paid the great majority of SUDs.
From my five years of experience, I can suggest if you are older, physically disabled, or have any serious financial condition.
Then Medicaid drug rehab will always be there to help you cover expenses and recover.
Let’s explore the blog and know-how, when, and where Medicaid covers your drug and alcohol rehab.
What Services Does Medicaid Cover for Drug and Alcohol Addiction?
Screening and Brief Intervention: Identifying Your Needs
The specialist identifies the severity of substance abuse and patterns of your individual needs. That involves alcohol testing, X-rays, detox, and so on.
Following the facts, the specialists are aware of the treatment. As well as guide and support you with necessary treatments after intervention with your close ones.
Medicaid may help you save $96 for half an hour for these.
Outpatient Treatment
Medicaid alcohol rehab gives the flexibility to continue your day routines while receiving counseling, therapy, and medical care. But before this, find out your rehab listed for Medicaid.
Click the link to find out some rehabs with Medicaid coverage in 2024.
Intensive Outpatient Treatment
Medicaid rehab coverage for intensive outpatient treatment (IOP), but remember it may vary with state and your treatment plan, including group therapy, individual counseling, and on and on.
Residential Treatment
Medicaid covers residential treatment.
This immersive atmosphere of Medicaid drug rehab offers rigorous therapy, counseling, medical care, and all the treatments you may need.
Medication-Assisted Treatment (MAT): An Unbeatable Path of Recovery
MAT is essential for opiate and alcohol addiction treatment. Medicaid rehab coverage covers methadone, buprenorphine, and naltrexone, which reduce cravings and withdrawal symptoms to help you stay sober.
Detoxification
Medicaid rehab coverage of medically supervised detoxification and safely managing withdrawal symptoms. That ensures a safe and comfortable transition at the initial state of treatment.
Counseling with Medicaid Rehab Coverage
Addiction treatment includes individual, group, and family counseling to help you address triggers, learn coping skills, and adopt better habits, which Medicaid pays for.
Aftercare
Medicaid alcohol rehab covers aftercare programs to stay sober and avoid relapse.
Are You Eligible for Medicaid? Track Your Treatment
My cousin applied for Medicaid to cover his drug rehab costs. We all know Medicaid helped 72.5 million natives.
The application process, I must say, was not without its hurdles as I helped him through this. However, common eligibility conditions we noticed are
Income Limits
Medicaid alcohol rehab targets low-income families and individuals where your family wage is under 133% of FPL (Federal Poverty Level). But the limit may vary by state, house hold.
Disability Status
Even if your income exceeds Medicaid income limits, Social Security Administration- or state-defined disabled people qualify for Medicaid.
Documentation You Need
Medicaid addiction treatment documentation varies by state and scenario to verify authentication. Commonly requested documents are-
Proof of Identity: Government-issued ID, Passport, Birth certificate.
Proof of Residency: Documents showing current address, such as utility bills, rental agreements.
Proof of Citizenship or Immigration Status: U.S. passport, Birth certificate, Alien registration card, Naturalization or Citizenship certificate.
Income Verification: Pay stubs, Tax returns, Bank statements, Supplemental security income or other income-related documents.
Apply for Medicaid
You can apply for Medicaid through your state’s Medicaid department or Healthcare. Apply online, in person, or by state medicaid agency.
Waiting Periods for Medicaid
Some states require a waiting period before determining Medicaid eligibility and activating benefits.
The period may differ depending on the population, facts of the service, and workers to give service to the state. It typically takes 45 days to proceed but may be delayed for lack of documentation.
However, Pregnant ladies and disabled ones can enroll immediately.
Key Differences
| Medicaid | Medicare | |
| Eligibility | Primarily for low-income individuals and families, certain elderly, and disabled individuals. | Generally for individuals aged 65 and older, some younger individuals with disabilities, and those with End-Stage Renal Disease (ESRD). |
| Funding | Funded jointly by the federal government and individual states. | Funded by the federal government through the Medicare program. |
| State Administration | Administered by individual states with federal oversight and guidelines. | Administered solely by the federal government. |
| Coverage | Offers a broad range of healthcare services and long-term care coverage, including drug and alcohol rehab. | Provides coverage for hospital services (Part A), medical services (Part B), and prescription drug coverage (Part D). Some individuals opt for additional private plans to cover gaps in coverage (Medicare Advantage – Part C). |
| Costs and Premiums | Costs and premiums vary based on state and individual circumstances. Some services may require copayments or cost-sharing. | Costs and premiums are standardized based on the specific Medicare plan chosen. Part A is generally premium-free for those who have paid sufficient Medicare taxes during their working years. |
| Enrollment | Enrollment is ongoing, and individuals can apply at any time, subject to eligibility criteria. | Initial enrollment is during the Initial Enrollment Period (IEP), usually around turning 65. General Enrollment Periods (GEP) and Special Enrollment Periods (SEP) are also for specific circumstances. |
| Long-Term Care | Provides extensive long-term care coverage, including nursing home care. | Offers limited coverage for skilled nursing facility care after a hospital stay (Part A) but not for custodial long-term care services. Individuals may need supplemental coverage (Medicaid or private insurance) for long-term care. |
One must understand Medicaid and Medicare to establish eligibility and get the right healthcare coverage.
Benefits of Using Medicaid Drug Rehab
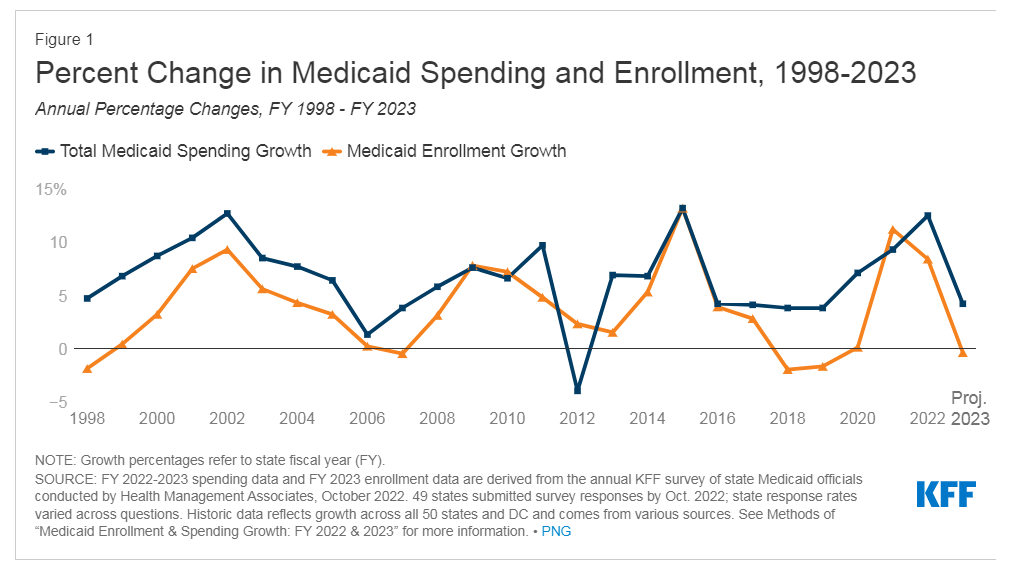
As an expert, I confirm Medicaid is remarkable for those who seek help but are financially unstable. Look at the chart. It speaks of Medicaid drug rehab benefits according to its spending versus enrolments-
I can also mention the benefits of using Medicaid for addiction treatment.
Source: KFF
Those are-
Financial Assistance
Medicaid assists those who cannot afford drug rehab. Medicaid helps low-income families afford healthcare, including drug and alcohol rehab.
Wide Range of Services : That You Must Know
Medicaid covers various drug and alcohol recovery therapies to meet individual needs.
Inpatient, outpatient, residential, detoxification, counseling, MAT, and aftercare include.
Multiple therapy techniques enhance the odds of discovering a good one.
Flexibility
Medicaid’s flexibility lets patients choose treatment venues and providers.
Beneficiaries can choose inpatient, outpatient, or residential programs depending on their needs and circumstances.
Holistic Medicaid Drug Rehab Care
Medicaid drug rehabs promote holistic treatment. That means your physical, emotional, psychological, and social causes are treated.
Holistic care treats you individually and improves well-being to increase recovery success and sustainability.
Continuum of Care
Medicaid provides continued support throughout the recovery process.
Medicaid-funded programs can provide complete care from detoxification and initial treatment to aftercare and relapse prevention, improving recovery results.
Access to Quality Care
State and federal quality criteria apply to Medicaid-approved drug recovery facilities.
Beneficiaries have access to recognized and accredited treatment facilities with qualified healthcare specialists.
Medicaid programs provide successful addiction treatment by following these guidelines.
People Also Asked
Can Veterans Qualify for Medicaid?
Yes, Medicaid eligibility depends on income and other variables, not military experience. Thus, veterans may apply.
Veterans who match their state’s Medicaid income and eligibility requirements can get Medicaid and VA healthcare.
How Long Does Medicaid Pay for Rehab?
Medicaid will cover the whole cost of nursing home care, including room and board, for as long as needed, even for life.
Does Medicaid Cover Substance Abuse Treatment?
Yes, Medicaid covers addiction therapy. Medicaid covers several behavioral health therapies, including drug rehab.
Outpatient therapy, MAT, detoxification, inpatient or residential treatment, and aftercare may be covered. Check with your state’s Medicaid program to determine what substance abuse treatment services are covered.
Does Medicaid Cover Inpatient Rehab?
Yes, Medicaid covers inpatient drug rehab.
Full-time inpatient rehab provides rigorous therapy and support. Inpatient alcohol rehab Medicaid services, including room and board, medical care, counseling, and other essential treatments, may be covered by Medicaid.
All Medicaid-covered services vary by state and scenario.
Does Medicaid Cover Rehab After a Hospital Stay?
Yes, Medicaid may cover post-hospital rehab.
After hospitalization, patients can get physical, occupational, and speech therapy with this coverage. Medicaid may cover substance misuse or mental health rehab if the hospital stay was related to those illnesses.
As always, state regulations and eligibility determine coverage.
Medicaid assists low-income, elderly, and disabled ones with drug and alcohol treatment. It includes screening, outpatient, inpatient, detoxification, counseling, and aftercare.
Medicaid supports recovery with comprehensive care and treatment flexibility. While coverage varies by state, it is a vital payer source that allows many Americans to get drug and alcohol addiction treatment.
- What to Pack for 30-Day Rehab? FREE Checklist - May 30, 2024
- Types of Outpatient Rehab: Difference One Should Know - March 28, 2024
- Truth Behind FMLA: Hidden Hurdles of Alcohol Rehab Leave - March 28, 2024